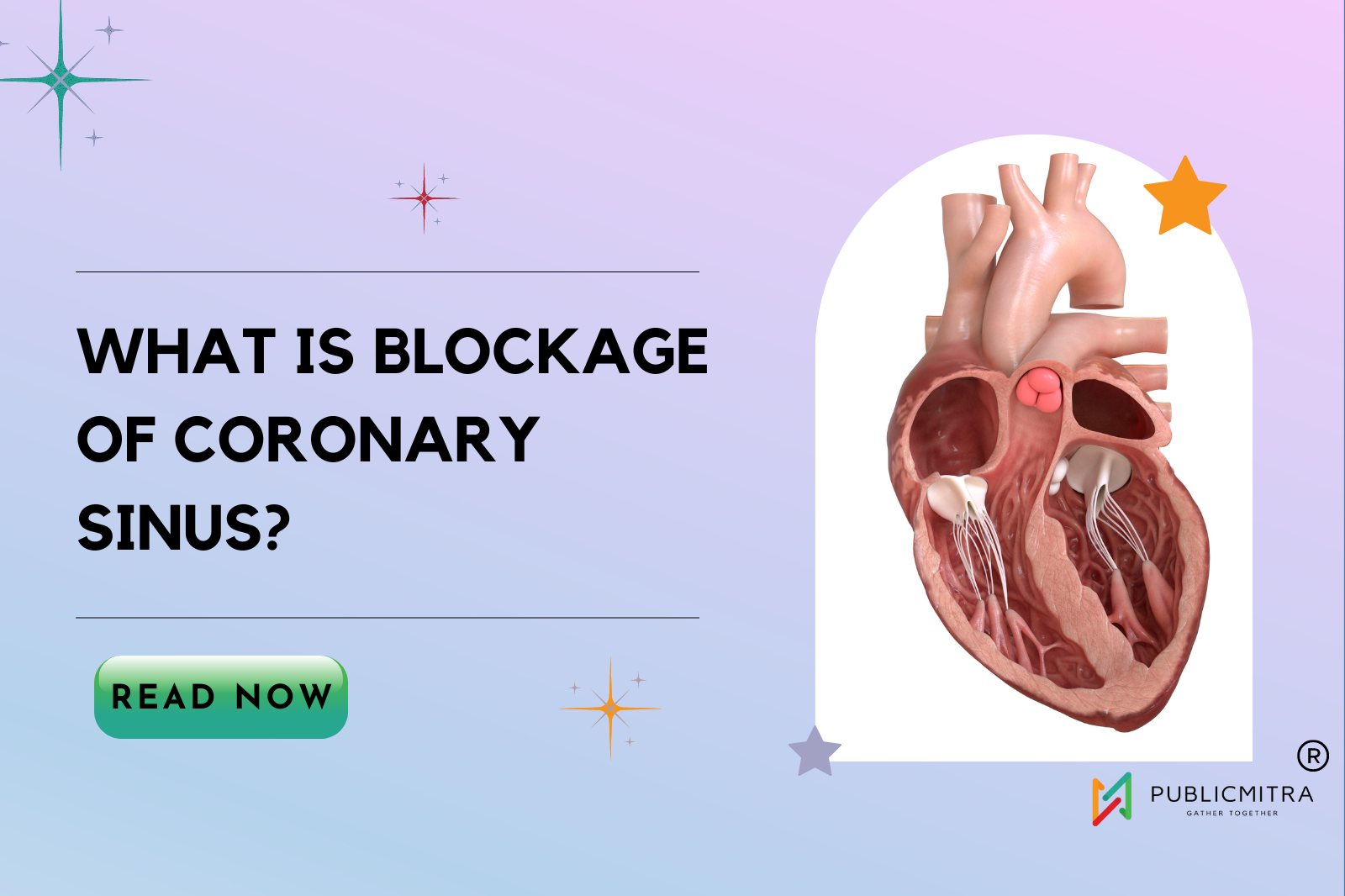
What Is Blockage Of Coronary Sinus?
What is the Blockage of Coronary Sinus?
In the cardiology domain, the coronary venous system plays a major yet often underestimated role. While coronary sinus thrombosis is a relatively rare occurrence, it can manifest as a severe complication, especially surfacing post-procedure. In this comprehensive review, let us understand the nuances of coronary sinus thrombosis, its causes, and treatment.
Unraveling CSOO
The coronary venous system is an intricate network of vessels within the cardiac anatomy. It assumes paramount importance in various cardiological procedures. Within this complex network lies the coronary sinus, a structure of pivotal importance that serves as the primary drainage vessel for venous blood from the myocardium.
CSOO, as the name suggests, is the obstruction or narrowing of the coronary sinus ostium, which is the entrance of the coronary sinus into the right atrium. This obstruction disrupts the normal blood flow within the heart. This is particularly concerning in patients with a single ventricle.
The Rarity of Coronary Sinus Thrombosis
Coronary Sinus Thrombosis (CST) is a condition characterized by the formation of blood clots within the coronary sinus. CST is a rare occurrence and is often associated with specific factors, the most notable being endothelial damage. This damage can occur as a result of invasive cardiology procedures, such as catheterization, or it may be triggered by underlying medical conditions. It may manifest either as a consequence of cardiovascular procedures or spontaneously, triggered by factors such as venous stasis and endothelial damage. While this condition may be regarded as an uncommon phenomenon, it should not be overlooked.
Causes of Coronary Sinus Blockage
Understanding the causes of blockage in the coronary sinus is crucial:
Endothelial Damage: Invasive cardiology procedures, which involve introducing catheters into the heart, can inadvertently damage the endothelial lining of the coronary sinus. This damage may create a favorable environment for clot formation.
Spontaneous Cases: In some instances, CST can occur spontaneously, without any prior cardiac procedures. These cases are often associated with factors like venous stasis (a slowdown of blood flow) or changes in the blood’s coagulation profile.
Underlying Heart Conditions: Patients with pre-existing heart conditions, such as atrial fibrillation or heart failure, may be at an increased risk of developing CST.
Complications that arise due to CST
Blockage of the coronary sinus can give rise to a cascade of complications:
Cardiac Tamponade: This is a severe condition where excess fluid compresses the heart, hindering its ability to pump effectively.
Myocardial Ischemia: A blockage in the coronary sinus can lead to reduced blood supply to the heart muscle, potentially resulting in tissue damage.
Pulmonary Embolism: Blood clots within the coronary sinus may dislodge and travel to the lungs, causing a pulmonary embolism.
Cardiac Arrest: In severe cases, CST can lead to cardiac arrest, a life-threatening condition where the heart ceases to function effectively.
Role of Diagnosis
CST presents a complex diagnostic challenge. Its symptoms are often vague and may mimic those of other cardiac issues. Patients experiencing CST may report chest pain, shortness of breath, or generalized weakness. Diagnosing this condition typically involves advanced imaging techniques, including computed tomography (CT) scans or echocardiography, to identify the presence of blood clots within the coronary sinus. At times, CST may be discovered incidentally during medical evaluations for unrelated concerns.
Echocardiograms: A Diagnostic Cornerstone
One of the fundamental tools in diagnosing CSOO is the echocardiogram. This non-invasive imaging technique provides great insights into cardiac structures and blood flow dynamics.
Key Diagnostic Clues
When interpreting echocardiograms in CSOO cases, clinicians should be attentive to specific findings:
Retrograde LSVC Flow: Retrograde flow in the left superior vena cava (LSVC) can be a telltale sign of CSOO.
Coronary Sinus Dilation: Dilation of the coronary sinus is another diagnostic clue that warrants investigation.
The Diagnostic Challenge
Diagnosing coronary sinus thrombosis is quite a challenge. This is where advanced imaging techniques come to the forefront, providing clarity in the diagnostic process. Multimodal imaging, encompassing computed tomography (CT), magnetic resonance imaging (MRI), and echocardiography, assumes a pivotal role in facilitating accurate and timely diagnosis.
Beyond Imaging
The clinical presentation of coronary sinus thrombosis is as diverse as it is elusive. Patients may present with a spectrum of symptoms, ranging from chest pain and dyspnea to palpitations and syncope. The manifestation often depends on the extent and location of the thrombus. Therefore, a meticulous clinical evaluation, coupled with a high index of suspicion, is crucial.
Treatment Strategies
The management of coronary sinus thrombosis traverses through uncertain waters, marked by a paucity of clear-cut guidelines. A multidisciplinary approach involving cardiologists, interventional radiologists, and hematologists is imperative in tailoring treatment strategies to individual patient profiles.
Anticoagulation
Anticoagulation therapy emerges as the cornerstone of treatment in most cases of coronary sinus thrombosis. The aim is to prevent further thrombus propagation and mitigate the risk of embolic complications. However, the choice of anticoagulant agent and duration of therapy remains a matter of clinical judgment, with patient-specific factors playing a pivotal role.
Thrombectomy
In select cases, especially those with extensive thrombus burden or hemodynamic compromise, thrombectomy may be considered. This invasive procedure involves the mechanical removal of the thrombus, often necessitating specialized expertise and equipment.
Potential Complications
Coronary sinus thrombosis is not without its dire consequences. Myocardial ischemia and pulmonary embolism are ominous threats, underscoring the need for prompt intervention and expert consultations. Early recognition and treatment are vital in averting these potentially life-threatening complications.
Coronary sinus thrombosis, though a rare entity, demands our unwavering attention and clinical acumen. The intricate interplay of causes, elusive clinical presentations, and nuanced treatment approaches underscores the need for an interdisciplinary approach. Collaboration between cardiology, radiology, and hematology specialists is pivotal in navigating the challenging terrain of coronary sinus thrombosis. As our understanding of this condition evolves, so too must our commitment to early recognition and optimized treatment, ensuring the best possible outcomes for our patients.
Wrapping up
In a world prone to single-ventricle heart disease, understanding and promptly addressing coronary sinus ostial obstruction (CSOO) is paramount. The cases discussed here underscore the significance of early detection and intervention. Echocardiograms, spectral Doppler LSVC interrogation, and selective angiography stand as essential tools in the diagnostic process.
This article has provided a detailed exploration of CSOO, its diagnostic intricacies, and the pivotal role it plays in the lives of patients with single-ventricle heart disease. Early detection, as exemplified in the infant’s case, can be a lifeline, while delayed diagnosis, as seen in the adult’s situation, presents significant challenges. It is our hope that this comprehensive overview contributes to the knowledge and awareness of this critical cardiac condition.